By Phoebe Ingraham Renda
Contrary to what a status quo hearing test would suggest, hearing involves more than ears—leaving some hearing difficulties undiagnosed. But now, University of Pittsburgh School of Health and Rehabilitation Sciences researcher Aravind Parthasarathy and colleagues have developed a diagnostic technique to uncover hidden hearing pathologies. It analyzes the brain’s response to sound with 30 times better resolution to assess hearing at every neurological level.
"We have not seen a new approach to hearing diagnostics in over 30 years,” says Catherine Palmer, professor of audiology and chair, Department of Communication Science and Disorders, School of Health and Rehabilitation Sciences. “Dr. Parthasarathy’s work supports targeting existing and emerging treatments to the people who will benefit based on their hearing loss characteristics.”

Aravind Parthasarathy, assistant professor of communication science and disorders, School of Health and Rehabilitation Sciences. Photography by Joshua Franzos.
What’s That Noise?
Traditional hearing tests only assess the inner ear's cochlear amplifier, which makes soft sounds louder and loud sounds softer in the first step of hearing. After the cochlear amplifier, sound travels through the auditory nerve, brainstem, cortex and the auditory neuronal pathway as the brain hears sound. As a result, pathological changes along that hearing path can trigger a neurological game of telephone.
“The next generation of hearing diagnostics should be a representation of what’s happening in your brain,” says Parthasarathy, assistant professor of communication science and disorders. “The idea is to assess things happening all along that auditory pathway.”
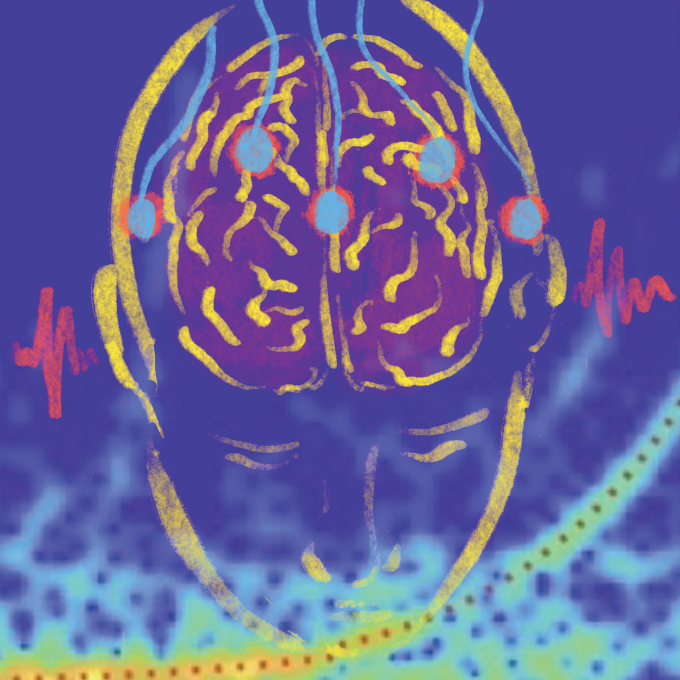
Adapted from electroencephalogram (EEG)-based technology used for newborn hearing screening, Parthasarathy’s diagnostic technique uses EEG electrodes placed on the scalp to detect the brain's electrical responses to sound.
“The cool thing about the hearing brain is that the neural responses directly mirror information in sound,” says Parthasarathy. “You can look for similarity between those sounds and the neural responses you get from the EEG.”
Analysis of those neuronal signals, Parthasarathy notes, can indicate if any parts of the brain are not responding to sounds as expected.
I Hear Your Voice, But Not Your Words.
Current hearing tests also do not reflect hearing in day-to-day life. Many patients report difficulty hearing others speak in noisy environments, like a restaurant’s din of clanging dishes, clinking tableware and overlapping conversations. However, in quiet clinical settings, these patients receive passing grades on their hearing tests, leaving them without a diagnosis. This “hidden” hearing loss may affect up to 10% of patients seeking help.
These perceived hearing difficulties, Parthasarathy notes, likely result from changes in how the brain processes information and sound along the auditory pathway. In their recent Nature Communications Biology publication, Parthasarathy and colleagues report on their promising diagnostic tool to detect hearing changes throughout the auditory pathway.
Parthasarathy’s diagnostic tool allows clinicians to objectively measure all stages of auditory processing by capturing how the brain neurologically represents the information in a sound. Additionally, the EEG technique collects robust neuronal-response data five times faster than established lab methods—making clinical integration easier.
While the diagnostic technique and its neuronal response analyses are still in early developmental stages, Parthasarathy and his team are working to connect different pathological conditions, like age-related hearing loss, metabolic stressors, like diabetes, and neurodegenerative diseases, like Alzheimer’s disease, to these neuronal sound response patterns.
“Once we have a model where we know the expected test responses from each of these pathologies, we can employ it in the clinic for patients with perceived hearing loss not captured by current clinical tests,” says Parthasarathy.
