By Michele Dula Baum
Discoveries about how genes influence health and disease have outpaced virtually every other avenue of scientific research since the Human Genome Project’s first sequence publication more than 20 years ago, leading to personalized treatment approaches for cancers and cardiovascular disease, and increasingly targeted drug development.
Genetics, however, make up just 5-8% of an individual’s health risk. Tools like artificial intelligence, machine learning, supercomputing power and big data are transforming the science of public health research into precision public health.
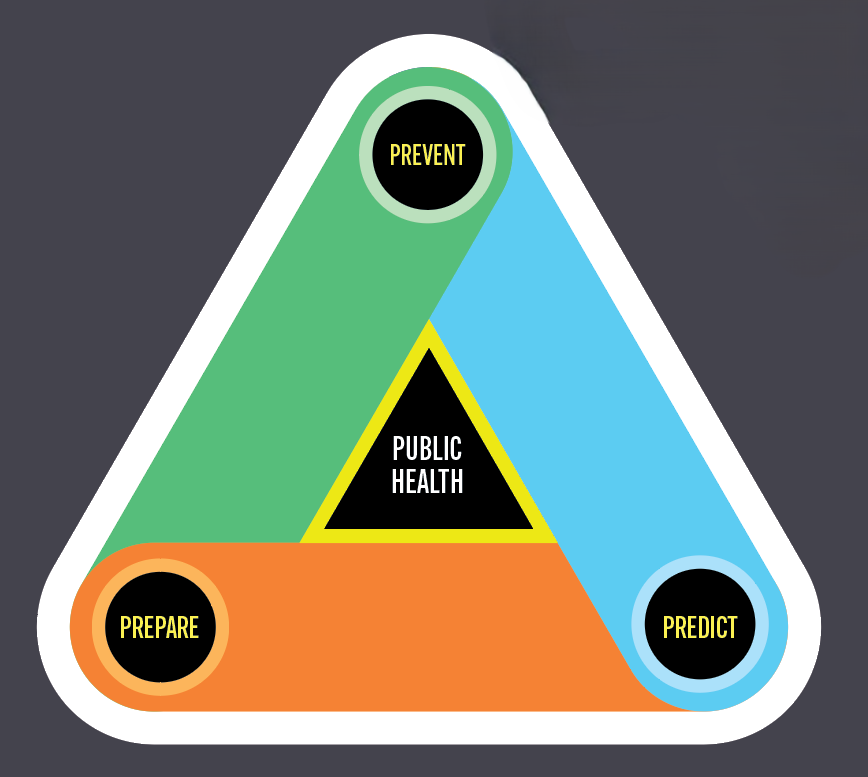
“Precision public health examines the collective influences of environment, lifestyle and genetics at the population level,” explains Maureen Lichtveld, dean of the University of Pittsburgh School of Public Health. “The goal is to predict, prepare and, ultimately, prevent disease in our communities.”
National health care expenditures are projected to reach $5.3 trillion in 2025 and are expected to exceed average gross domestic product growth by 2032, according to the U.S. Centers for Medicare and Medicaid Services. Some 90% of those costs are for people with chronic and mental health conditions, according to the Association of Schools and Programs of Public Health.
Research consistently confirms that public health initiatives are associated with reduced emergency room visits, hospital stays and overall mortality. Community-based programs keyed to mental health, nutrition and substance abuse also lower long-term health care expenses.
“An individual’s ZIP code is a better predictor of their future health outcome than their entire genome. We can think of that as a starting point for precision public health to target better health outcomes in our communities,” notes Anantha Shekhar, senior vice chancellor for the health sciences and John and Gertrude Petersen Dean, School of Medicine. “Why is this ZIP code worse than the one that’s one or two miles away?”
The creation of the United States Public Health Service in 1873, followed by state, municipal and county health departments, promoted nutrition and hygiene, better waste management, pure drinking water and, in time, conducted disease surveillance to help prevent the spread of illness.
“Powerful 21st-century data analytics tools like machine learning and artificial intelligence are key components of a precision public health approach to predicting future disease threats and effective mitigation,” says Suresh Kuchipudi, professor and chair of infectious diseases and microbiology, Pitt Public Health.
New infectious diseases continue to emerge, bringing with them threats to human health. HIV and SARS CoV-2, the novel coronavirus that causes COVID-19, first arose in animals, circulating through other species before becoming transmissible to humans.
“We’re doing a much better job with some of the new genomic tools we’ve got, but artificial intelligence is going to allow us to do a lot with big data analysis and a lot more cross talking with social determinants of health risk factors, exposure and genetic risk factors—to the extent that we can use those tools effectively,” says Georges Benjamin, executive director of the American Public Health Association.
“On a population level in so many ways, it’s really just a new way to think about doing what we’ve always done, but in a more targeted way,” Benjamin adds.
Excerpt provided from Pitt Public Health magazine's Spring 2025 issue.
