
From left to right: Castanha, Burke, Marques
Pitt researchers developed a new synthetic biomarker technology to distinguish between prior Zika and dengue infections within individuals. By analyzing blood samples from infected individuals, the researchers were able to pinpoint specific biomarkers that accurately differentiate between the two viruses, which are cross-reactive, meaning that an immune response to one can also flag an immune response to the other, making it difficult to tell which virus is causing, or previously caused, infection. The technology may lead to the development of better diagnostics and vaccine candidates, scientists announced in the Proceedings of the National Academy of Sciences.
Until now, researchers and clinicians have lacked diagnostic tools to easily differentiate between prior infections with different flaviviruses, a family of mostly mosquito- and tick-borne viruses that include Zika and dengue.
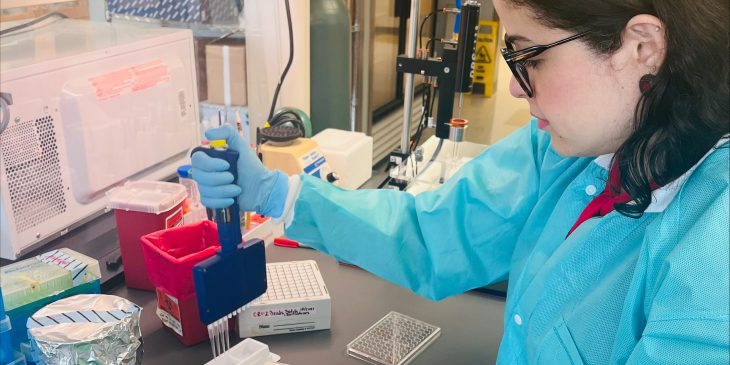
Photo credit: Amro Nasser
Antibodies for Zika virus can be confused in many diagnostic tests with antibodies for dengue virus, making it difficult to tell if someone who tests positive previously had dengue, Zika or both. “This makes it very difficult to test new treatments or determine how widespread an emerging disease may be in areas endemic for flaviviruses, which cause a high burden of illness globally,” said first author Priscila Castanha, assistant professor of infectious diseases and microbiology at Pitt Public Health.
It is especially important for reproductive-age women to know if they already had Zika—and likely have immunity—because infection during pregnancy can cause birth defects. Knowing if they have immunity or not could guide the extent of people’s efforts to avoid mosquitoes in endemic areas during pregnancy.
The crossdisciplinary research team used an approach pioneered by cosenior author Thomas Kodadek, a chemist with The Wertheim UF Scripps Institute. The study was funded by the National Institutes of Allergy and Infectious Diseases and used a combination of advanced computational modeling and experimental techniques to identify distinct molecular structures associated with Zika and dengue infections.
“The technology is amazing. You don’t need to know the sequence, or the structure, or even the pathogen,” said cosenior author Donald Burke, Pitt Public Health dean emeritus. “As long as you have chosen the right sets of patient blood samples to compare, you can tease out the important antibodies that differ between the patient sets, along with the corresponding synthetic molecule biomarkers.”
Castanha, Burke and cosenior author Ernesto T.A. Marques, associate professor of infectious diseases and microbiology at Pitt Public Health, have been studying Zika virus since it emerged in the Americas in 2015. Prior to its emergence in Brazil, Castanha, Marques and Burke were studying dengue virus.
“For every sample we tested during the 2015 outbreak, we had to do 10 different blood tests to confirm Zika,” said Castanha. “These tests are technically difficult and time-consuming, making them impractical for providing clinical guidance. I think if we had this molecule back then, it would’ve been fantastic.” With precise differentiation between the two viruses, clinicians can make more informed decisions regarding patient treatment and management strategies.
Importantly, the new synthetic biomarker technology doesn’t require refrigeration, “making it particularly useful for outbreaks occurring in remote or low-resourced areas,” said Kodadek.
The technology could be expanded to other infectious diseases, offering a versatile, reliable platform for diagnostic innovation and research and, ultimately, improved patient outcomes.
